In Europe the incidence and severity of CDI is increasing,[1],[2],[3],[4] with nearly 125,000 cases a year,[5] posing a major threat to healthcare systems and patientsData presented today from the CDI Service Evaluation study shows that the adoption pattern of treatment impacts CDI outcomes. Compared to traditional broad-spectrum antibiotics, first-line use of fidaxomicin - a targeted treatment - in all CDI patients provides the best outcomes in terms of recurrence rate, all-cause mortality and cost effectiveness, compared to use in selected patients only.[6] CDI is associated with high-mortality[7] and cost burden,[8] therefore reducing the incidence and recurrence of CDI is a priority for clinicians, payers and health authorities alike.
Over 1,450 patients were included in the analysis conducted in seven UK hospitals that introduced fidaxomicin, a narrow-spectrum antibiotic for the treatment of CDI, between July 2012 and July 2013.[6] Data collected from 177 patients treated first-line with fidaxomicin during the 12-month evaluation period were compared with those from a retrospective cohort treated with broad-spectrum antibiotics - vancomycin and metronidazole - during the previous 12-month period.[6]
In the two centres (A and B) where fidaxomicin was adopted as a first-line treatment for all patients diagnosed with CDI, a significant reduction in 28-day all-cause mortality was observed, from 18.2% to 3.1% (P<0.001) and 17.3% to 6.3% (P<0.05) respectively.[6],[9] The real-world analysis also supports clinical trial data in highlighting dramatically reduced recurrence rates: from 12.1% and 23.5% with vancomycin and metronidazole, to 3.1% in both centres with first-line fidaxomicin. For every 50 patients treated, this would result in 5 and 10 recurrences avoided in the two centres respectively.[6]
A separate study recently looked at the impact of CDI treatment on environmental contamination. The analyses showed those treated with fidaxomicin are more than 20% less likely to contaminate their environment with CDI (36.8%) compared to patients treated with metronidazole and/or vancomycin (57.6%). This significant decrease in environmental contamination may further contribute to a reduction in secondary cases of CDI.[10]
“The European Society of Clinical Microbiology and Infectious Diseases (ESCMID) identified recurrence as the next big challenge to be met in the treatment of CDI, since it occurs in up to 25% of patients treated with current broad-spectrum therapies,” comments Professor Mark Wilcox, Professor of Medical Microbiology, Leeds Teaching Hospitals & University of Leeds. “Fidaxomicin has limited activity against the ‘good bacteria’ in the gut and so can be considered to be a targeted treatment option. Preservation of the gut microflora likely contributes to the lower rates of recurrence seen after fidaxomicin treatment of CDI compared with those associated with broader-spectrum antibiotics like vancomycin.”
A CDI recurrence has been previously estimated to add an additional £20,249 on top of an estimated £13,146 spent to treat the initial infection due to prolonged hospital stay, ICU stay, high cost drugs and the surgery necessary to tackle it.[11] An in-depth costing analysis at the two centres that adopted fidaxomicin as a first-line treatment revealed that in centre A the 5 recurrences that could be avoided for every 50 patients treated with the narrow-spectrum antibiotic would result in a cost saving of £19,490, and in centre B, for the 10 recurrences avoided, a cost saving of £121,144.[6] With nearly 125,000 cases of CDI occurring in Europe each year,[5] the potential cost saving for the treatment of this potentially fatal condition is likely to be far greater.
The cost-effectiveness of fidaxomicin has been reinforced in a recent study in France, with fidaxomicin proving to be both clinically and cost-effective compared to vancomycin.[12] The main driver of cost-effectiveness was a significant reduction in the rate of recurrence, resulting in a reduced cost of hospitalisation.[12] In the base case, fidaxomicin was cost-effective compared to vancomycin for all patients at a cost per QALY of €24,242.[12] The cost per recurrence avoided was €1,877 and cost per faecal transplant avoided was €8,967.[12]
In Europe the incidence and severity of CDI is increasing, posing a major threat to healthcare systems and patients.[1],[2],[3],[4] Information suggests that CDI results in death for 9% (2% primary cause, 7% contributory) of all diagnosed patients.[7] This suggests that CDI contributes to the death of around 27,000 people each year across Europe,[7] around five times that of MRSA associated deaths.[13]
ESCMID guidelines currently recommend DIFICLIR as a first line therapy option in CDI patients at risk of recurrence and in patients with severe and non-severe CDI.[14]
NOTES TO EDITORS
About the CDI Service Evaluation study[6]
The CDI Service Evaluation Project is the first and only real-world multicenter study assessing the effectiveness of current CDI treatment for UK patients in NHS Secondary Care Trusts in England. This evaluation looked specifically at the cost-effectiveness of fidaxomicin in clinical practice versus standard of care treatments (vancomycin and metronidazole) in seven trial centres from across the UK:
• Leeds Teaching Hospitals NHS Trust
• Guy’s and St Thomas’ NHS Foundation Trust
• County Durham & Darlington NHS Foundation Trust
• University Hospitals of Morecambe Bay - NHS Foundation Trust
• St George’s Healthcare NHS Trust
• University Hospitals of Leicester NHS Trust
• Derby Hospitals NHS Foundation Trust
The study was sponsored by Astellas Pharma Ltd.
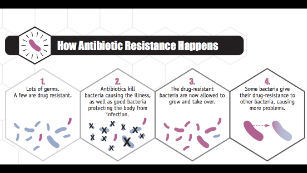
About Clostridium difficile Infection
CDI is a recurring and preventable illness resulting from infection of the internal lining of the colon by C. difficile bacteria.[15] The bacteria produce toxins that cause inflammation of the colon, diarrhoea and, in some cases, death.[16] Patients typically develop CDI after the use of broad-spectrum antibiotics that disrupt normal bowel flora, allowing C. difficile bacteria to flourish.[17] CDI is highly infectious[18] and has surpassed MRSA as a leading cause of healthcare-acquired infection.[19] It is most common in those taking broad-spectrum antibiotics that result in the disruption of normal bowel flora,[20] and threatens those most vulnerable, including the elderly, patients who are immunocompromised or with renal impairment and those who have prolonged periods of hospitalisation.[21],[22] People in hospital with CDI are up to three times more likely to die in hospital (or within a month of infection) than those without CDI.[23],[24] Information suggests nearly 125,000 cases of CDI occur in Europe each year,[5] and that CDI results in death for 9% (2% primary cause, 7% contributory) of all diagnosed patients.[7] Recurrence of CDI occurs in up to 25% of patients within 30 days of initial treatment with current therapies.[25],[26],[27] The ESCMID has identified recurrence as being the most important problem in the treatment of CDI.[28]
About DIFICLIR (fidaxomicin)
DIFICLIR (fidaxomicin) is a first-in-class macrocyclic antibiotic targeted to kill the C. difficile bacteria[29] while sparing the ‘good’ gut bacteria,[30],[31],[32] and represents the newest development in CDI for over 20 years.[33],[34] In the largest Phase III trials in this area fidaxomicin was shown to be non-inferior in initial cure and clearly superior to current standard of care treatment - vancomycin - in achieving sustained clinical cure and addressing recurrence.[27],[35] ESCMID guidelines recommend DIFICLIR as a first line therapy option in CDI patients at risk of recurrence and in patients with severe and non-severe CDI.[14] The safety profile of DIFICLIR is based on data from 564 patients with CDI treated with fidaxomicin in Phase III studies.[33]
About Astellas Pharma EMEA
Astellas Pharma EMEA operates in 40 countries across Europe, the Middle East and Africa, and is the EMEA regional business of Tokyo-based Astellas Pharma Inc. Astellas is a pharmaceutical company dedicated to improving the health of people around the world through the provision of innovative and reliable pharmaceuticals. The organisation’s focus is to deliver outstanding R&D and marketing to continue growing in the world pharmaceutical market. Astellas presence in Europe also includes an R&D site and three manufacturing plants. The company employs over 4,500 people across the EMEA region. In 2013 Astellas was awarded SCRIP Pharmaceutical Company of the Year in recognition of its commercial success and pipeline development.